Being in the hospital gives me PTSD.
Like actual PTSD. My breathing is shallow and fast, I start feeling trapped and claustrophobic. I sweat. The really smelly kind of sweat. My mind fills with a torrent of fear that drowns out all other thoughts.
And to my horror, when I get angry at not being heard, I cry. When the tears burn down my face, I become even angrier that I’m crying and less able to speak up.
This is why when I told my husband a year ago that we were going to have a baby, I also told him I’d like to have our baby at home. He was already familiar with most of my hospital traumas, including the discovery that I’m allergic to two common medications—after they were pumped into my IV. Twice.
I’ve been rushed into emergency surgery 3,000 miles away from home and I’ve spent a week as a medical test subject. I also have the type of veins phlebotomists dread. It takes three sticks on average for a needle to find a suitable spot. I once sprayed a two foot stream of blood across a wide-eyed nurse.
After a month or so of petitioning for a home birth, he finally agreed and we found the most extraordinary midwife. We had a healthy pregnancy and a dream birth at home. Six hours of calm in a safe space with no medical intervention and full-on mindful breathing resulted in a healthy, happy, eight pound, 15 ounce bundle of joy.
All of our intentional avoidance of hospitals has now flown right out the window.
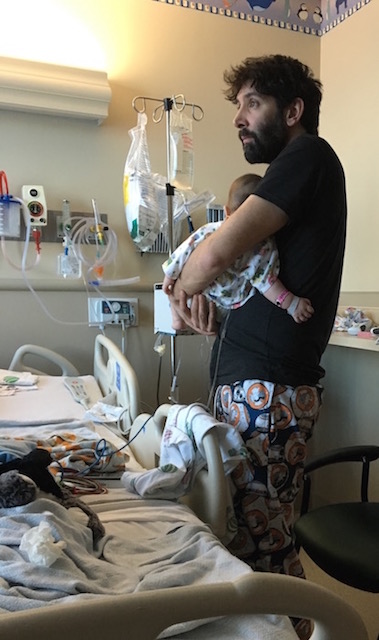
Today is my second day in the pediatric ward hovering over my three month old son as he struggles to breathe. It’s taken me two days, two long exhausting days to wake up. Entering the hospital through the Emergency Room is like being placed on a moving sidewalk. I’m whisked away before I even realized that I was no longer standing still.
Two days ago when my husband and I first noticed our son seemed to be having a hard time catching his breath, I immediately worried his bad cold had migrated down into his chest. I’ve had pneumonia and both my husband and I have asthma. It seemed remote, and my new mom instincts were a little overreactive as of late.
A month-and-a-half ago we drove to the Emergency Room on a Saturday evening because I was worried our little one had a cold/pneumonia/croup/
Sometime after we got home I remembered that I may have accidentally sprayed the little one up the nose with breast milk when he unlatched during an exhaustive feeding session during the previous night. Breast feeding can be challenging. The sniffle went away in about a day.
So when two days ago I said, “We’re going to Urgent Care, now,” my husband somewhat rightly looked a little hesitant. Instead of arguing or rolling his eyes, he acknowledged what I thought were chest retractions while we were bathing our baby, and helped me bundle him up and into the car.
After an RSV diagnosis and being told to immediately go to the ER by the physician assistant at Urgent Care, we found ourselves whisked into glaring fluorescent lights and a cold sterile room. My meditation training, my yogic training, my physical performance training all seemed to go into hibernation the moment I walked through the germ splattered doors of the hospital. Alternating between interminable waits and frenetic activity quickly brought on the PTSD.
My husband ushered me out of the room the first two times the nurses and phlebotomist tried to put an IV line into our little one. I stood outside the room near the nurses’ station and cried heaving sobs into my hands as I listened to my sweet, normally serene little boy scream in fear and pain. One of the nurses asked if it was my baby and when I nodded without looking up, she sighed sympathetically and said, “It must be your first.” As if it gets easier with subsequent children.
Although I couldn’t seem to think mindfully myself, each time I gathered my little one into my arms to comfort and calm him, I started with a deep breath. “Let it out sweet boy. Deep breath,” as I inhaled deeply and exhaled slowly.
After the fifth IV placement, with an oxygen cannula attached to his face, and vital monitor hanging from his foot, there was hardly a place on our little one’s body that didn’t ache or have a bandage. For the next 48 hours we obsessively checked his oxygen levels in between nebulizer treatments and tried to make him as comfortable as possible in his vast hospital bed. My husband brought a few blankets and stuffed animals from home to lessen the impersonal feel of the room as we watched and waited.
I’m embarrassed to say for those first two days I hadn’t even thought about my contemplative practice. Neither sitting meditation, movement, nor breathing exercises outside of deep breathing to calm my son even occurred to me. Watching and counting breaths should have triggered 13 years of training. I let the PTSD overwhelm my senses in the blur between hourly nurse rounds, respiratory specialist treatments, and occasional pediatrician visits. The nurse down in the ER was right. I recoiled from my little one’s cries each time he was held down to have his nose suctioned, before preparing to pick him up afterwards and comfort him while swallowing my own tears.
It took me two days of watching my son wrestling with each breath before I remembered to take a breath of my own. With my husband’s firm encouragement, I ventured out of our room for the first time. Armed with a medical mask to protect our son from the germs of the hospital and the other pediatric patients from his RSV, I shuffled along the linoleum floors in my slippers. I hadn’t realized how stiff I had become. I was hunched over and exhausted from the past two days. I finally breathed. Deep breaths that sucked my yellow mask into my mouth. I watched my slow steps and tried to remember the cues from my walking meditation training.
When I came back into the room after dousing myself in hand sanitizer, my chest was lighter. My body had unfurled finally and I could stand up straight. My son greeted me with his big smile. The silent giggle one that crinkles his eyes and shows the pink gums where teeth soon will be.
While walking down the hospital hallways, I realized that being here for my son’s sake has alleviated some of my own fears and allowed me to work through my PTSD triggers. He can’t speak up for himself, but I can. When the stress of meeting so many strangers and having so many treatments overwhelms him, I’m here to ground him. To hold him. To love him. To let him know he isn’t alone.
The pediatrician just stopped by and told us that we get to go home tomorrow.
While I hold my sleeping little one with the whirring and beeping monotonously droning on, I’m thinking about venturing back out into the world. I hope to continue remembering to breathe. It’s easy to try to become a martyr for our little ones. It’s hard to remember the importance of creating the space for our own breaths. Parenting is full of fearful moments, but breathing carries us through.
I’m also starting to wake up and notice that my mindfulness practice isn’t for the easy days. I practice so that when the world is spiraling out of control, I can find refuge. A soft spot to land. My practice might not always look like it had before. For me, becoming a mother has been the most revolutionary way of practicing contemplativeness and beginner’s mind. When I feel exhausted and wrung out, our little one is teaching me to slow down. He currently likes to look at inanimate objects that I’ve never noticed before. I recently followed his gaze and spent a whole minute contemplating our bedroom light fixture. It really does refract the light beautifully.
When we go home tomorrow, I’ll try to remember to breathe. To know that mindfulness will creep in when I need it most. It may not look the way I think it should, but it will remind me to slow down. To sit with my fears. It took long enough, but while counting my son’s breaths in the pediatric ward, I finally found my own again.
~
~
~
Author: Kenni Linden
Image: Courtesy of Author
Editor: Travis May






Read 1 comment and reply