An IMPORTANT for any service providers; in all capacities everywhere there is human interaction.
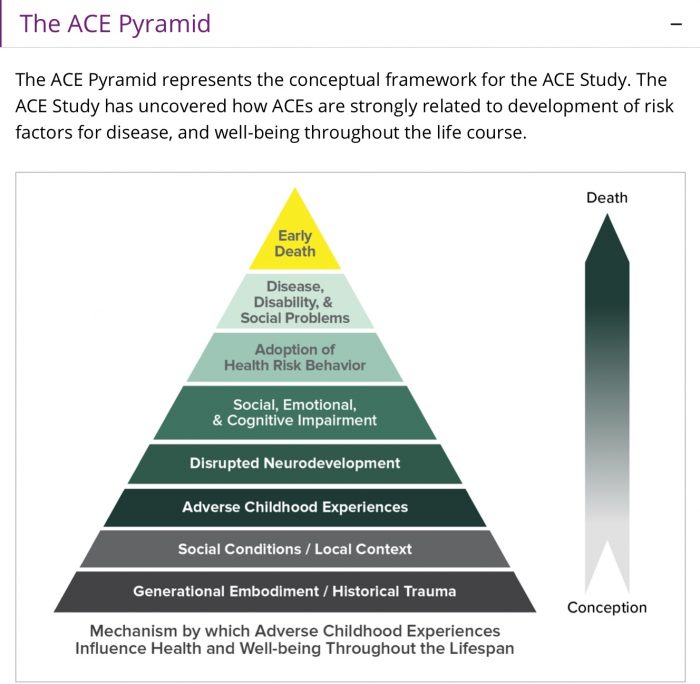
I’d like to discuss the ACE STUDY which has been defined as “ the single greatest threat to future health outcomes affecting our nation.”
Yet 23 years later, we still are not, addressing the compelling evidence and It’s staggering!
Besides the most recent stats, that suggest 1 in 3 girls and 1 in 6 boys will experience some form of sexual assault before the age of 18 yrs of age and 93% of child sexual abuse victims will KNOW or have some form of a relationship with their abuser, and that those who live through sexual assault are about more than 4x as likely to experience PTSD as adults – it doesn’t end with only adversely affecting mental health as one might I already know, nor does it only begin with sex crimes. It’s far more common than that.
In 1997, Kaiser Permeate published the results of extensive research into Adverse Childhood Experiences, with the outcomes documented in the ACE Study.
That study, like the impact of lead poisoning, second hand smoke, poor nutrition etc has the capacity to change, most everything we think we know about the risk factors of future illness, has been ignored despite being indisputable!
23 years later, few outside of humanities and social sciences, know the full extent of the data or even use the study as a screening tool…..And many EVEN in psychiatry still think ACE infers to a direct correlation to those taboo abuses – and It does not!
It’s far bigger and a wider net to cast, and yes it’s frightening!
Here are foundation points, for predictable long term health outcomes .. ( hold onto your hats – a child’s future health outcomes rests heavily on this criteria – much of which we cannot control but it’s still of incredible importance no less. )
Copied below from ACE Study data 1995-97 – Science, without prejudice and not my words.https://www.cdc.gov/violenceprevention/childabuseandneglect/acestudy/index.html
All ACE questions refer to the respondent’s first 18 years of life: Every answer of yes, is a score of 1 – they add up quickly, even in what we deem as “ normal” families!
Abuse:
-Emotional abuse: A parent, stepparent, or adult living in your home swore at you, insulted you, put you down, or acted in a way that made you afraid that you might be physically hurt.
-Physical abuse: A parent, stepparent, or adult living in your home pushed, grabbed, slapped, threw something at you, or hit you,,that you had a mark or may have been were injured.
-Sexual abuse: An adult, relative, family friend, or stranger who was older than you, has ever touched or fondled your body in a sexual way, made you touch his/her body in a sexual way, attempted to have any type of sexual relations or intercourse with you.
Household Challenges:
-Mother treated violently: Your mother or stepmother was pushed, grabbed, slapped, had something thrown at her, kicked, bitten, hit with a fist, hit with something hard, repeatedly hit for at least a few minutes, or ever threatened or hurt by your father (or stepfather) or your mother’s boyfriend.
-Substance abuse in the household: A household member was a problem drinker or alcoholic or a household member used illicit drugs or other maladaptive vices to cope.
-Mental illness in the household: A household member was depressed or mentally ill or a household member attempted suicide.
-Parental separation or divorce: Your parents were ever separated or divorced.
Incarcerated household member: A household member went to prison.
Neglect
-Emotional neglect: Someone in your family helped you feel important or special, you felt loved, people in your family looked out for each other and felt close to each other, and your family was a source of strength and support.
-Physical neglect: There was someone to take care of you, protect you, and take you to the doctor if you needed it, you didn’t have enough to eat, your parents were too drunk or too high to take care of you, and you had to wear dirty clothes.
*Verbatim and not my description.*
The ACEs Study of adverse childhood experience ranks childhood trauma as any of the above as a precursor- calling it an “epidemic” that poises the” single greatest unaddressed threat to mental and physical health in our world.”
Survivors of childhood trauma as per described above, with an ACE score of 4 or more criteria, have a significantly INCREASED risk of physical disease in adulthood, including cardiovascular disease, autoimmune disease, chronic illness, degenerative disease, premature aging diseases and CANCER ( not including all the Mental Health challenges) and a 20 year shorter life expectancy than those with ACE score of zero!
A 20 year shorter life expectancy! Take a minute to let that sink in.
Now one would think that if we knew this ( which we do ), great efforts would go into courses for new parents with basic psycho-social education, become a part of pre-natal classes, it would be a mandatory class in lifestyle and Phys Ed classes and become a mainstream screening tool in every physician’s office across the nation, especially paediatricians – where they have the tools for early intervention to cope with childhood trauma’s before they become post-traumatic health disorders and yet this is NOT standard practice.
The evidence is overwhelming, terrifying and yet remains for the most part; unaddressed!
My mission beyond writing and speaking is to bring trauma-informed care to every institution and profession, that is based in customer service.
Since my Shrink Rap Radio video podcast, I’ve been asked by many to come speak and train service providers, from bartenders and hairstylist to lawyers and dentists. We all need to be trauma informed, unless we work in isolation behind a computer screen where there is absolutely no human contact whatsoever and yet they still go home to relationships.
Trauma Informed Care should be considered a universal precaution, as simple as hand washing before serving someone in your aesthetician’s chair, to staff in the emergency room.
We wash our hands to avoid spreading germs and infection, it’s precaution for the client, the provider and the general population.
As service providers working with fellow human beings – we must be aware of the impact of trauma and how it affects both one’s physical health, mental health, their relationships and it impacts on their life choices, situations and their most basic of activities of daily living.
The evidence is indisputable and yet, for the most part, we have ignored the data.
I have my own theories as to why this is and there are many but the one key reason I see is DISCOMFORT and that’s simply a poor excuse, ONCE we KNOW the statistics.
Many are uncomfortable – I’m sorry, I’m not sorry. Life is complicated.
Many think trauma informed care means asking the client to re-live and re-tell a narrative that may cause great discomfort for both the client and the service provider, that is not what it means at all.
It’s actually quite simple – presume!
When a patient goes into a walk in clinic with a cough and fever, we don’t know, until they have been assessed, whether or not they have a virus, the flu, pneumonia or whooping cough but we take precautions just in case….it’s presumed that everyone IS contagious until we know otherwise – BEFORE removing the precautionary mask.
Trauma Informed care, is a precaution, a presumption, that assumes everyone has a trauma history and treats them accordingly, for safety reasons amongst so many others.
It’s not rocket science, but people still feel awkward and resistant to embracing a model of care and compassion that can only ENHANCE the professional relationship, between client and provider of any and all services; not just medical.
Here are two recent examples from my own personal experience in the last few months where having trauma-informed training could have made a world of difference – massage therapy and emergency dentistry.
Have you ever been to a massage therapist and filled out one of those lengthy questionnaires? Mine recently was 3 pages long with a detailed Q&A of my health, medications and predispositions or medical history of certain illnesses and cancers that are familiar; that may carry a strong genetic predisposition or run in one’s family like breast or colon cancer. Symptoms of mental health syndromes, are asked like depression or anxiety but there was no box to tick for trauma! I find this astounding, that it’s not considered important to know.
Consider how difficult it may be for someone with a trauma history, to disrobe, get naked or almost naked, lay face down on a table and allow a complete stranger to touch them all over their bodies, in a darkened room, for up to an hour or longer for a full body massage.
Or at the dentist – where unless I am in excruciating pain, I never go. All the sedatives available to calm my dental phobia which has nothing to do with a phobia, cannot touch the level of activation stemming from my fight or flight response, it’s hard to tranquilize my body as it rises.
When I am laid back in a chair, being told not to move, while a stranger is in full control, where I feel frozen, where objects far too big for my mouth like even an X-ray is inserted, before then being frozen and having my mouth violated with drills; swished with a chemical cocktail of antiseptics, and foreign objects, while I remain still and unable to speak or sit up, without it being potentially dangerous.
I have had sit downs over the years with various dentists to explain my phobia is far bigger than irrational fear and anxiety, and often it’s been meant with confusion as to how the to how one is even remotely linked to the one another.
Until I met my current dentist and his dental assistant who both admitted to receiving absolutely no trauma informed training in college or in medical school. It was a light bulb moment as he called it, that offered a new explanation as to why it’s more typical then not, to receive daily cancellations and no shows.
The solution simple – ASK.
Not for details but the simple question of where or not that client has a trauma history and what they can do to help make the experience less triggering and more bearable…. We practiced this as I panicked before my root canal and extraction.
After a brief description of trauma Informed care, we tried it out:
Dr. T: “ Is there anything that our staff can do to make this experience today, feel safer for you, given your history?”
Me: “ Yes, 3 things : 1. Ask me for a nod of consent before you begin each step, then explain to me exactly what you are doing and approximately how long each step may take. 2. Don’t sensory overload me with background small talk, leave the TV over the chair off, it doesn’t distract me, it adds to the feeling of chaos. 3. If I raise my hand, it means I need to take a break for even a few seconds, and if doing so, may be unsafe at that moment, tell me that, and when that task is over – let me sit up.”
Easy question with simple requests, and no presumption that my requests are the same as another survivor’s.
Every one is different so ASK EVERYONE! Many prefer the distractions. Know the client and their needs, we are all different.
I cannot begin to tell you what a world of difference this has made for both of us.
One of my many past dentists was so anxiety ridden when I sat in his chair that his hand shook – it was not good for either of us. He compared it to “ first month dating nerves” – that didn’t help either.
He meant no ill intent, he simply didn’t know any better, because no one had ever tought him otherwise.
Now that this dentist knows, he uses it for everyone and guess what?
Less medications and less cancellations.
Everywhere in life’s interactions, there is often an imbalance of power even if it seems as ever so minor as one’s hairstylist or mortgage broker, one must in seemingly unremarkable ways, hand over their power, even when it’s not being taken from you.
Surrendering control of our finances or our hair to another person with scissors can feel threatening, even if it’s not.
So who needs trauma Informed care in practice? Everyone!!!!
Who especially needs it? Law enforcement, lawyers, judges, clergy, coaches, therapists and anywhere the imbalance of power feels that much greater.
Preventatively, it begins with new parents and should be a mandatory requirement at birth, to know how our behaviours and what seems like our personal stories, directly impact our ability to parent effectively and knowing the long term ramifications of our actions, even those we cannot control, and how they impact a developing young mind.
Most importantly, it needs to become a mainstream screening tool for predictable future health outcomes, in every physician’s office, across the globe, just like routine physicals, and new patient consultations.
This is the place where trauma should safely be addressed and dealt with accordingly, to prevent future disease processes including post-traumatic stress disorder, which says in the first word “ post” or delayed reaction because it was not properly addresse, in the first place.
We can’t prevent traumatic experiences, but we have the capacity to prevent further harm done by them and why we aren’t doing it remains a mystery and is inexcusable.
#nomore. It’s beyond time – we all get educated ❤️







Read 0 comments and reply